A comprehensive food waste progam for a typical 1,000 bed hospital can be carefully designed to become successful and sustainable.
Nicole Chardoul and Beth Coddington
BioCycle September 2012, Vol. 53, No. 9, p. 29
Americans throw away an estimated 40 percent of the total U.S. food supply. Hospitals are a major contributor to this waste stream, with food waste making up 10 to 15 percent of the 6,600 tons of waste they dispose each day.

A typical 1,000-bed hospital reported serving over 8,600 meals/day. Over half were patient meals, and the rest divided between the main cafeteria, small food service vendors and the doctors’ dining room.
The first step in planning a comprehensive hospital food waste program is to examine the waste generated — where it comes from and how much there is. Although hospital food and nutrition managers often first look towards the kitchen, food and other organic wastes are actually found throughout the hospital: in cafeterias and other dining areas; break rooms and lounges; and at special events. A typical 1,000-bed hospital reported serving over 8,600 meals/day, over half of which were patient meals, and the rest divided between the main cafeteria, smaller food service vendors and the doctors’ dining room. Other sources of organics included paper towel waste from bathrooms and yard trimmings from the landscaping department.
After tracking down sources of organic waste, the next step is to quantify it. A waste characterization should look at amounts of viable food for donation, compostable organic waste from pre and postconsumer sources, nonrecyclable paper streams and yard trimmings. An actual waste sort is one option, looking at a one- or multiple-day sample of waste from food service areas to determine the percentage of potentially recyclable and compostable waste.
If a full waste sort is not possible, a visual estimation can be done by observing loads of trash for a period of a few weeks, noting the percentage observed to be food waste, and comparing that to the actual weights of dumpsters or compactors for the same period. Standard metrics also can be used to estimate the amount of divertible waste: 4 to 10 percent of food purchases in a commercial setting become waste before ever reaching the consumer. In cafeterias approximately 0.5 lbs. of food waste is generated per meal tray. For a sample hospital, a waste study found approximately 0.31 lbs of food waste was generated per meal served across all locations.
Recovery Options
Armed with a fuller understanding of the sources and volumes of food waste, a hospital’s next steps are to design a program incorporating both waste reduction and recovery elements. Inside the hospital, food service operations are complex, involving multiple vendors, preparation areas for patient and visitor food services, different types of reusable or disposable tableware in different areas of the hospital, and a variety of disposal operations post-meal, ranging from staffed conveyor belts to tray return racks to unmanned trash areas. Even in a typical hospital using some reusable dishware, an array of disposable products such as cups, plates, trays, condiments and Styrofoam for hot drinks and soups for patient meals are common elements of the waste stream. Because of these complexities, a recovery plan has to address how pre and postconsumer food waste would be segregated from noncompostable waste, how to minimize contamination from the disposable tableware in use, and how to store and transport compostable waste through the hospital building.
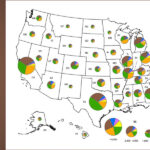
The critical step in designing an institutional composting program, however, is not so much managing the internal logistics of the program but rather determining what to do with the organics once collected. Many hospitals would like to compost food waste, but there is a lack of local facilities permitted to accept organics along with yard trimmings. In Southeast Michigan, for example, the market for food waste composting has developed rapidly over the past six years with specialized trainings, support from the Department of Environmental Quality, FAQs, etc. Some yard trimmings composting sites are now accepting food wastes — some with compostables products and some without — thus increasing opportunities for off-site processing. But the options remain slim and many institutions looking for a hauler to transport their food waste to a permitted processing facility find this is largely an unmet market.

A one-day sort of waste from food service areas helped determine the percentage of potentially recyclable and compostable waste.
the hospital grounds maintenance staff, in an on-site greenhouse or sold to employees and visitors at an on-site farmer’s market. Other hospitals have collaborated with local food growers and farm managers to utilize their food scraps for composting or animal feed.
Sample Rollout
A sample rollout program designed for a hospital with over 1,000 beds in southeast Michigan includes three main elements. First, based on results of the waste sort, food and disposable tableware purchases will be reduced to eliminate waste. Second, an existing food donation program will continue to provide the highest and best use for foods that were prepared but not served. Finally, an off-site composter will process remaining food waste: pre and postconsumer vegetative wastes; cooked food; meat, bones and dairy; and napkins, compostable plates, cups and utensils. Rollout will take place in three phases, each focused on one area of the hospital. Based on the results of the waste sort, the hospital could anticipate having 0.83 tons/day of food waste in the first phase of rollout, and up to 1.32 tons/day once the program is fully rolled out.
The first phase of the program focuses on the kitchens, patient meals and the tray return line. Types of waste include prep waste and table scraps from patient meals. To avoid contamination, noncompostable disposable products will be eliminated from patient meals so everything left on the trays will be china, silverware or made of compostable materials such as paper.
The second phase adds in food from the cafeteria and staff lounges, requiring several additional process changes to food service operations. Disposable products will need to be converted to durable dishware to avoid contaminating the compostable materials with plastic containers. Instead of single serve condiments in noncompostable packets, bulk condiment dispensers will be used. “To-Go” products and premade sandwiches and salads will be packaged in compostable materials. The end result of these changes is that the vast majority of waste generated in the cafeteria and lounges will be compostable, resulting in little contamination in the compostable bin in these areas.
In the third phase of the program, other food service and “grab and go” operations will be converted to compostable materials, with trash bins converted to labeled compostable bins to collect this waste stream. A final optional stage of the program would add in soiled paper such as paper towel waste and soiled cardboard. While posing some challenges in collection, the addition of these materials would help reduce odor, absorb moisture in collection containers, and allow more air to circulate.
The compost rollout plan addresses four main issues regarding impacts of the program. First, to minimize the effects on dining and waste collection operations, the program was designed to work with the unique space constraints of each location. Existing 32-gallon containers will be repurposed to collect food waste, lined with clear, compostable liners. Dedicated rolling carts can be used for food waste pickups within the hospital.
Second, the high costs of compostable products posed an immediate challenge to actual program implementation. Indeed, the cost of compostable serviceware exceeded that of standard disposables by 132 percent, on average, and some product such as liners cost 200 percent more. However, this cost impact can be mitigated through a reduction campaign in which customers are given reusable dishes unless to-go containers are specifically requested. As a large percentage of disposables are simply used in the cafeteria then thrown out on site, a full switch to compostables under this new system would increase costs by 14 percent, rather than 132 percent.
Third, potential for compost bin odors were addressed by planning for the food waste dumpster to initially be emptied on a daily basis. Unless odor from this dumpster is unmanageable, the pick up frequency can then be adjusted to every other day to reduce hauling costs. A cart wash system, either by the hauler or at the hospital, is also being considered to keep the bins clean.
Finally, in launching a compost program in a large facility, contamination is an ever-present worry. Different strategies must be used for areas where contamination can be easily monitored, including kitchens and tray returns, versus those difficult to control, such as cafeterias and lounges. For the latter, the best ways to combat contamination are through purchasing — making sure the majority of waste generated in the cafeteria will be suitable compostable material, signage and education, and continued oversight and engagement by all staff responsible for elements of the program.
Total cost of the program, including the switch to compostable serviceware, is estimated at $597,000 annually. However, costs will also be avoided, including purchases of noncompostable disposable products, and reduced trash hauling and disposal charges. Thus, the net increase over current costs for a full program rollout is approximately $87,000 annually (Table 1). Additional savings are possible through source reduction in the kitchens and food preparation areas. The program will divert 13 compactor loads (125 cy/compactor) from the landfill each year, avoiding greenhouse gas emissions of 387 metric tons CO2 equivalent.
Nicole Chardoul, P.E., is Principal and Vice-President of Project Operations with Resource Recycling Systems (RRS) in Ann Arbor, Michigan. Beth Coddington is an RRS consultant.